Skull Base Tumours, Tumours of the Jugular Foramen (Glomus Tumours)
Surgery of the skull base, sometimes more formally referred to as surgery of the cranial base, is a relatively new development. Skull base surgical techniques are directed at tumours which cross the base of the skull whereby they involve not only the bone of the skull itself but also the cranial cavity and its contents and the upper part of the neck and associated aerodigestive tract. These tumours are rare and, although usually benign, formerly were almost always fatal. Modern surgical treatment has revolutionised the outlook.
Symptoms
The symptoms and signs caused by tumours of different areas of the skull base:
- Intermediate skull base (greater wing of the sphenoid)
- Headache; Visual disturbance; Diplopia; Trismus; Facial numbness; Loss of the corneal reflex.
- Posterior skull base (jugular foramen)
- Pulsatile tinnitus; Conductive hearing loss; Lower cranial nerve palsies; Sensori-neural hearing loss and vertigo (late); Headache (raised intracranial pressure).
- Central skull base (clivus chordoma)
- Headache; Diplopia (sixth nerve); Facial numbness
Surgery of the Skull Base
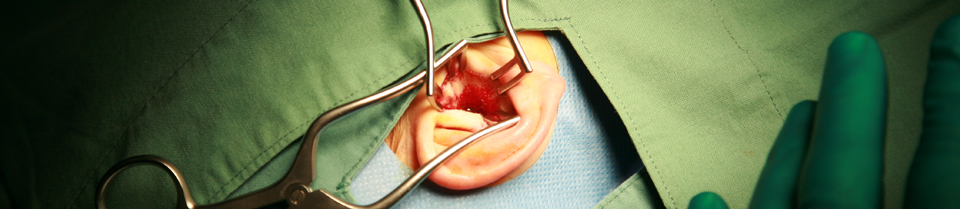
Skull base surgery is best defined as the systematic removal of bone, to give access to extensive tumours in the adjoining areas.
Surgical procedures for the removal of skull base tumours are extremely lengthy. It is not unusual for a jugular foramen tumour to require six to eight hours of surgical time for removal. Of necessity, recovery is prolonged. The major postoperative problems are those related to the loss of cranial nerves, in particularly the lower cranial nerves (IX to XII).
Skull base tumours untreated are nearly always lethal. Treatment requires a team representing the disciplines of otology, head and neck surgery, neurosurgery, radiotherapy, radiology and speech pathology as well as experienced theatre staff and nursing staff. St Vincent’s has developed a team of excellence in the Surgery of Skull Base Tumours with experience of over 100 cases.
In most patients with skull base tumours these days, a return to normal or near-normal quality of life with normal life expectancy can be anticipated.
Selected publications:
Fisch U, Fagan PA, Valvanis A (1984) “The Infratemporal Fossa approach to the Lateral Skull Base”, Otolaryngol Clin of North America 17: 3, 513-552.
Grattan-Smith JD, Doust BD Fagan PA (1988) “High Resolution Computer Tomography in the Evaluation of Glomus Tumours of the Petrous Temporal Bone” Austral Radiol. 32: 190-196.
Biggs MT, Fagan PA, Sheehy J, Bentivoglio P, Doust BD, Tonkin JP: (1991) “Meningioma of the Posterior Skull Base”. Skull Base Surg. 1: 43-50.
Fagan PA, Sheehy J Bentivoglio P, Tonkin JP, Berg D, Sheridan BF, Jensen J: (1992) “Surgery of the Skull Base – A Review of 70 Cases” Med J Aust. 156: 717-721.
Buchanan DS, Fagan PA, Turner J (1992) “Cavernous Haemangioma of the Temporal Bone”, J Laryngol Otol. 106: 1086-1088.
Fenton JE, Brake H, Shirazi A, Mendelsohn MS, Fagan PA(1996) “The Management of Dysphagia in Jugular Foramen Surgery” JLO 110: 141-147.
Fagan PA(1996) “Tumours of the Skull Base” Mod Med Aust. Aug: 66-74.
Fenton JE Brake H Shirazi A, Mendelsohn MS, Fagan PA (1996) “The Role of Lower Cranial Nerves in Jugular Foramen Surgery” Acoustic Tumour and Skull Base Surgery, Proceedings of the Second International Conference on Acoustic Neuroma Surgery, Paris, France, Kugler Publications, New York.
Fagan PA (1996) “Tumours of the Skull Base” Mod Med Aust. Aug: 66-74.
Fenton JE Brake H Shirazi A, Mendelsohn MS, Fagan PA (1996) “The Role of Lower Cranial Nerves in Jugular Foramen Surgery” Acoustic Tumour and Skull Base Surgery, Proceedings of the Second International Conference on Acoustic Neuroma Surgery, Paris, France, Kugler Publications, New York.
Chang P Fagan PA Roche J (1997) “Imaging Destructive Lesions of The Petrous Apex”, Laryngoscope 107: 1-7.
Turner J, Chang P Noushi F Fagan PA (1998) “Aggressive Papillary Tumour of the Temporal Bone – New Immunohistochemical Evidence of Endolymphatic Sac Origin” Aust J Otolaryngol 3: 50-56.
Chang P, Fagan PA Roche J (1998) “Imaging Destructive Lesions of the Petrous Apex” Laryngoscope 108: 599-604.
Patino-Cordoba JI Turner J McCarthy SW Fagan PA (1998) “Chondromyxoid Fibroma of the Skull Base” Otolaryngol Head and Neck Surg. 118: 415-418.
Wijetungia L.H. Raj, Fagan PA, Sheehy JP, (1998) “Petrous Apex Meningiomas: An Alternative Surgical Approach” J Clin Neursc 5:3 310-317.
Lavy J, Turner J, Cole IE, Fagan PA (2000) A Skull Base Approach to Chondroblastoma on the Cranial Bones” Aust J Otolaryng 3:504-507
Biggs ND, Fagan PA, Cole IE, Sheridan B (2001) “The Lateral Skull Base Approach to Extensive Nasopharyngeal Tumours” Aust J Otolaryn 4:1 33-37.
Liu R, Becvarosvki Z, Fagan PA Turner J, Adler J (2001) “Verrucous Carcinoma of the Temporal Bone” Aust J Otolaryn 4:1 56-58.
Jansen J, Turner J, Sheehy JP, Fagan PA, (2003) “Recurrent Rhabdoid Meningioma: Case Report”, Skull Base, 13: 51-54.
Rodrigues S, Fagan PA Turner J (2004) Endolymphatic Sac Tumours: A review of the St Vincent’s Hospital Experience, Otol and Neuro-Otol 25:599-603
Badenhop RF, Jansen JC, Fagan PA, Lord RSA, Wang ZG, Foster W J, Schofield PR (2004) “The prevalence of SDHB, SDHC and SDHD mutations in patients with head and neck paraganglioma and association of mutations with clinical features” JH Med Genet 41 e 99 (www.jmed,qenet.com/cfli/content/full/41/7/e99)
Arts A, Fagan Pa, (1991) “Vagal body Tumours”, Otolaryngol Head Neck Surg. 105:76-85
If you would like more information on Skull Base Surgery to be sent to you click here.
See also St Vincent's Ear, Acoustic Neuroma, and Skullbase Courses for clinicians.
