Management of Vestibular Schwannoma (Acoustic Neuroma) Research Study
Management of Vestibular Schwannomas and other Skull Base Tumours
The department has been running a prospective study of the management of Vestibular Schwannomas and other skull base tumours over the last 10 years. The following is an outline of the study. If you would like further information regarding the study please contact Dr Sean Flanagan, A/Prof Nigel Biggs or Dr Phillip Chang.
Background
A vestibular schwannoma is a benign tumour arising on the eight cranial nerve, the nerve of hearing and balance. Whilst this tumour is benign, its close proximity to vital neural structures can lead to serious complications, including death. The commonest presenting symptom is one of hearing loss, but disturbances in balance, as well as other sensory abnormalities are not uncommon. Diagnosis is usually confirmed on MRI or CT scan.
Vestibular schwannomas represent 80% of all CPA tumours. The other pathologies found here include meningiomas, facial schwannomas, epidermoids, lipomas, haemangiomas and metastatic lesions.
Traditionally the management of all these tumours was with intra-cranial micro-surgery. Current management options now include micro-surgery, stereotactic and conservative management, which involves serial imaging and clinical reassessment.1-3 Some patients then progress onto interventional therapy if they fail conservative management either related to progressive growth or progression of symptoms. A small proportion of patients will require revision surgery, surgery following radiotherapy and radiotherapy following surgery. Difficult management decisions surround the timing of intervention, the attempt to preserve function including hearing, and the patients co-morbid state.
The aim of this study is to accumulate a balanced set of data that will allow us to determine the optimal management paradigm.
Standard outcome measures have included hearing, facial function, vestibular or balance function, rates of CSF (brain fluid) leak and mortality figures. 4-7 8,9. In recent years there has been an increasing move toward assessing more holistic outcomes of management. This predominantly involves the use of well validated patient health surveys, or Quality of Life Surveys. 6,10-19.20-23
Up until this point in time our data base has collected information regarding patient demographics, tumour site, size, and operative details.
The aim of the study is to analyse outcomes of management and the use of quality of life questionnaires will provide us with additional, otherwise difficult to quantify consequences of the management and natural history of these tumours.
Participant eligibility
There are four non-randomised patient cohorts currently recognised.
1. Firstly the group of patients with vestibular schwannoma who following diagnosis were treated with surgery or radiotherapy.
2. The second group are those who were, and continue to be treated by observation.
3. The third group are those who during their period of conservative management failed this modality, necessitating surgical or radiotherapeutic intervention.
4. Those patients requiring additional treatment following surgery or radiotherapeutic treatment.
Recruitment and consent process
Patients diagnosed with a vestibular schwannomas (or other skull base tumours or lesions) are offered the opportunity of enrolling in the study. The management of vestibular schwannomas is a tertiary referral condition, and as such a significant number of patients have initially been diagnosed by another physician and then referred to one of the members of the St Vincent’s Department of Otolaryngology, Head and Neck and Skull Base Surgery
Eligible patients will be introduced to the study and given information regarding the study at their clinic appointment. The information provided to patients regarding the study will include; a cover letter with a Participant Information Sheet and Consent Form, the 5 study questionnaires and a symptom ‘summary sheet’ to complete.
Methodology
The data collected is patient name, date of birth, presenting symptoms and date of onset. This specifically includes: hearing calculated using a pure tone average and speech discrimination score in both ears, examination of vestibular function, facial nerve function reported using the House-Brackman scale, and the presence or otherwise of tinnitus, trigeminal symptoms and evidence of raised intracranial pressure. The initial doctor seen is recorded, and consequently the doctor overseeing their treatment if different. The size of the tumour as reported on an MRI scan, divided into its intracanalicular and cerebellopontine angle components is noted. Standard non-invasive vestibular tests are also employed. This includes Video Head Impulse Test or “VHIT”, vestibular evoked myogenic potential tests OVEMP and CVEMP, videooculography VOG and vestibulospinal tests of the balance pathways24-26. If clinically indicated caloric tests of vestibular function will be performed and recorded.
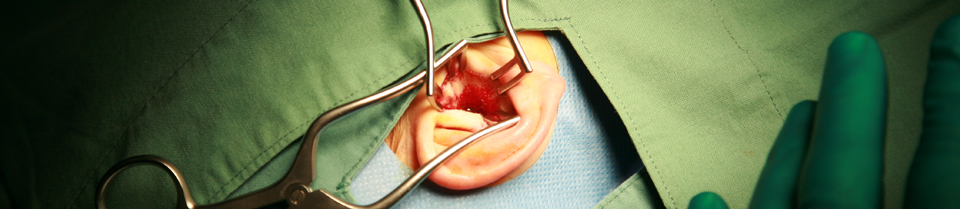
In terms of intra-operative data: the hospital at which surgery is performed, primary and secondary surgeon, approach used, total time, facial nerve function in recovery (House Brackman scale27), time spent in ICU, time in hospital, presence of post-operative complications. Follow-up data includes changes in the parameters already recorded.
From a radiotherapy perspective, the modality used, total dose given, number of fractions and presence of post-treatment complications. Follow-up data includes changes in the parameters already recorded.
5 quality of life instruments are part of an attempt to obtain global data of how a patient responds to the diagnosis and ongoing management of their tumour.
Historically the most widely used instruments have been the Glasgow Benefit Index GBI, and the SF-36, in addition to a number of self designed questionnaires. The GBI is purely designed as a post-interventional tool11,18 so is not appropriate for our study. The SF-36 is the other commonly used tool, but in previous studies two main weaknesses have developed. The first is the single administration, usually at an arbitrary period following intervention. For a condition with a long natural history, and especially in those patients managed conservatively, the change in QOL is far more important to measure. The second factor is it’s generality. The addition of two specific QOL instruments we propose will allow us to isolate the most important factors influencing the overall QOL.
The QOL instruments we are using are firstly the SF-36, a well validated general quality of life survey. The remaining instruments are the Hearing Handicap Inventory 14,28 , the Dizziness Handicap Inventory 29,30 and Tinnitus Handicap Inventory,31 all specific tools with close relevance to the disease process being studied. We also propose to use the PANQOL, (Penn State University Acoustic Neuroma Quality of life Survey) which is a disease specific validated survey. 21,32 Each questionnaire is expected to take less than five minutes to complete.
The timing of administration of these questionnaires is important in order to minimise bias. The questionnaires will be administered by direct post, in the first instance one month following initial diagnosis of a vestibular schwannoma. Follow-up administrations will on average each twelve months, independent to the treatment undergone. Previous use of the HHI and DHI has been isolated to patients treated with surgery, with an initial pre-operative assessment, followed by 3 or 6 months post-operatively. There have been no reports of their use in those managed conservatively. Similarly the SF-36 has only been used (in this setting) as a single administration. 17,19 .
Collection and storage of tumour samples
If patients should ever require surgery for their schwannoma or other skull base lesion, details regarding the type of surgery, how long the surgery took and their post operative course will also be collected as well as details about exact nature of schwannoma that was removed. Tumour samples will then be kept in the department of anatomical pathology and may be used for future research. Any future research conducted on tumour samples collected for this project will require separate Human Research Ethics Approval.
References
1. Lee JD, Park MK, Kim JS, Cho YS. The Factors Associated With Tumor Stability Observed With Conservative Management of Intracanalicular Vestibular Schwannoma. Otol Neurotol 2014.
2. Huang X, Caye-Thomasen P, Stangerup SE. Spontaneous tumour shrinkage in 1261 observed patients with sporadic vestibular schwannoma. J Laryngol Otol 2013;127:739-43.
3. Telischi FF, Morcos JJ. Vestibular schwannoma: evidence-based treatment. Otolaryngologic clinics of North America 2012;45:xvii-xviii.
4. Friedman RA, Kesser B, Brackmann DE, Fisher LM, Slattery WH, Hitselberger WE. Long-term hearing preservation after middle fossa removal of vestibular schwannoma. Otolaryngol Head Neck Surg 2003;129:660-5.
5. Sanna M, Khrais T, Russo A, Piccirillo E, Augurio A. Hearing preservation surgery in vestibular schwannoma: the hidden truth. The Annals of otology, rhinology, and laryngology 2004;113:156-63.
6. Walsh RM, Bath AP, Bance ML, Keller A, Rutka JA. Consequences to hearing during the conservative management of vestibular schwannomas. Laryngoscope 2000;110:250-5.
7. Raut VV, Walsh RM, Bath AP, et al. Conservative management of vestibular schwannomas – second review of a prospective longitudinal study. Clinical otolaryngology and allied sciences 2004;29:505-14.
8. Samii M, Matthies C. Management of 1000 vestibular schwannomas (acoustic neuromas): hearing function in 1000 tumor resections. Neurosurgery 1997;40:248-60; discussion 60-2.
9. Vivas EX, Wegner R, Conley G, et al. Treatment outcomes in patients treated with CyberKnife radiosurgery for vestibular schwannoma. Otol Neurotol 2014;35:162-70.
10. Sandooram D, Hornigold R, Grunfeld B, Thomas N, Kitchen ND, Gleeson M. The Effect of Observation versus Microsurgical Excision on Quality of Life in Unilateral Vestibular Schwannoma: A Prospective Study. Skull Base 2010;20:47-54.
11. Sandooram D, Grunfeld EA, McKinney C, Gleeson MJ. Quality of life following microsurgery, radiosurgery and conservative management for unilateral vestibular schwannoma. Clinical otolaryngology and allied sciences 2004;29:621-7.
12. MacAndie C, Crowther JA. Quality of life in patients with vestibular schwannomas managed conservatively. Clinical otolaryngology and allied sciences 2004;29:215-8.
13. Ryzenman JM, Pensak ML, Tew JM, Jr. Patient perception of comorbid conditions after acoustic neuroma management: survey results from the acoustic neuroma association. Laryngoscope 2004;114:814-20.
14. Humphriss RL, Baguley DM, Axon PR, Moffat DA. Change in hearing handicap after translabyrinthine vestibular schwannoma excision. Otol Neurotol 2004;25:371-8.
15. Baguley DM, Humphriss RL, Axon PR, Moffat DA. Change in tinnitus handicap after translabyrinthine vestibular schwannoma excision. Otol Neurotol 2005;26:1061-3.
16. Humphriss RL, Baguley DM, Moffat DA. Change in dizziness handicap after vestibular schwannoma excision. Otol Neurotol 2003;24:661-5.
17. da Cruz MJ, Moffat DA, Hardy DG. Postoperative quality of life in vestibular schwannoma patients measured by the SF36 Health Questionnaire. Laryngoscope 2000;110:151-5.
18. Nikolopoulos TP, Johnson I, O’Donoghue GM. Quality of life after acoustic neuroma surgery. Laryngoscope 1998;108:1382-5.
19. Baumann I, Polligkeit J, Blumenstock G, Mauz PS, Zalaman IM, Maassen MM. Quality of life after unilateral acoustic neuroma surgery via middle cranial fossa approach. Acta oto-laryngologica 2005;125:585-91.
20. Wangerid T, Bartek J, Jr., Svensson M, Forander P. Long-term quality of life and tumour control following gamma knife radiosurgery for vestibular schwannoma. Acta neurochirurgica 2014;156:389-96.
21. Robinett ZN, Walz PC, Miles-Markley B, Moberly AC, Welling DB. Comparison of Long-term Quality-of-Life Outcomes in Vestibular Schwannoma Patients. Otolaryngol Head Neck Surg 2014.
22. van Leeuwen BM, Herruer JM, Putter H, Jansen JC, van der Mey AG, Kaptein AA. Validating the Penn Acoustic Neuroma Quality Of Life Scale in a sample of Dutch patients recently diagnosed with vestibular schwannoma. Otol Neurotol 2013;34:952-7.
23. Carlson ML, Tveiten OV, Driscoll CL, et al. Long-term quality of life in patients with vestibular schwannoma: an international multicenter cross-sectional study comparing microsurgery, stereotactic radiosurgery, observation, and nontumor controls. Journal of neurosurgery 2015;122:833-42.
24. Halmagyi GM, Weber KP, Aw ST, Todd MJ, Curthoys IS. Impulsive testing of semicircular canal function. Progress in brain research 2008;171:187-94.
25. Iwasaki S, Chihara Y, Smulders YE, et al. The role of the superior vestibular nerve in generating ocular vestibular-evoked myogenic potentials to bone conducted vibration at Fz. Clin Neurophysiol 2009;120:588-93.
26. Kinoshita M, Iwasaki S, Fujimoto C, et al. Ocular vestibular evoked myogenic potentials in response to air-conducted sound and bone-conducted vibration in vestibular schwannoma. Otol Neurotol 2013;34:1342-8.
27. House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1985;93:146-7.
28. Jacobson GP, Newman CW, Monsell E, Wharton JA. False negative auditory brainstem response findings in vestibular schwannoma: case reports. Journal of the American Academy of Audiology 1993;4:355-9.
29. Pollock BE, Driscoll CL, Foote RL, et al. Patient outcomes after vestibular schwannoma management: a prospective comparison of microsurgical resection and stereotactic radiosurgery. Neurosurgery 2006;59:77-85; discussion 77-85.
30. Jacobson GP, Newman CW. The development of the Dizziness Handicap Inventory. Archives of otolaryngology–head & neck surgery 1990;116:424-7.
31. Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Archives of otolaryngology–head & neck surgery 1996;122:143-8.
32. Shaffer BT, Cohen MS, Bigelow DC, Ruckenstein MJ. Validation of a disease-specific quality-of-life instrument for acoustic neuroma: the Penn Acoustic Neuroma Quality-of-Life Scale. Laryngoscope 2010;120:1646-54.
See also St Vincent's Ear, Acoustic Neuroma, and Skullbase Courses for clinicians.
